Lule and Nolens
Prof. John Lule and Dr. Mrs. Barbara Nolens
Dutch gynaecologist Barbara Nolens started working in Mulago hospital (Uganda) in 2012, after she finished her specialization in obstetrics. One of her projects is Mama Mulago: to improve maternal health and neonatal outcome. Together with prof. John Lule, she will present the following:
Preventing unnecessary caesarean sections by reintroduction of the vacuum extraction, the story of Mulago hospital.
Obstetrics, Mulago Hospital Kampala, Uganda
Introduction
Obstructed labour is one of the five major causes of maternal mortality in low resource settings. Vacuum extraction can prevent or treat obstructed labour and hereby prevent maternal and perinatal morbidity and mortality. According to the WHO, vacuum extraction is one of the seven critical functions of basic emergency obstetric care. However it is hardly used in sub-Sahara-Africa. Less than 1% of deliveries is by vacuum extraction, compared to 10% in, for example, the Netherlands. Our program aims at increasing the vacuum extraction rate in Mulago Hospital, by providing equipment and training staff. Increasing the vacuum extraction rate will have the following benefits: It reduces the need for caesarean section and the risks that accompanies surgery. A reduction in caesarean sections implies faster maternal recovery and saving of resources. An unscarred uterus reduces the risk of uterine rupture, placenta praevia and accreta in future pregnancies. A shorter decision to delivery interval will lead to better fetal and maternal outcomes. Furthermore doctors trained in this university hospital will take their skills to all parts of Uganda after graduating.
Setting:
Mulago Hospital is a tertiary referral hospital and the university teaching hospital for Makerere University, Kampala, Uganda. It has over 31.000 deliveries per year, with many of them being complicated referrals. Every year 20 gynaecologists and 50 doctors (medical officers) graduate from this university hospital.
Methods:
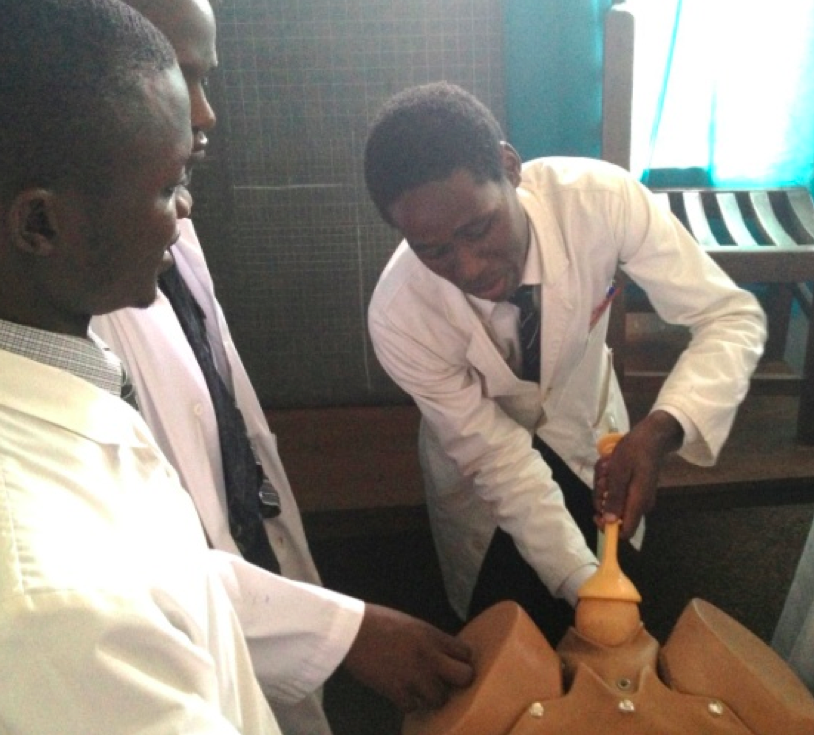
In November 2012 we provided vacuum extraction equipment and trained the 45 residents in obstetrics and gynaecology in Mulago Hospital. Training consisted of theory, hands on skills training on a mannequin and on the job training.
Results:
The use of vacuum extraction increased from 0.1% to 3.9% of deliveries. In 19 months 860 vacuum extractions were performed. Many caesarean sections were prevented. The perinatal mortality decreased significantly, mainly because of a decrease of 15% in the fresh stillbirth ratio.
Discussion:
Our program to reintroduce vacuum extraction to Mulago Hospital has many benefits. It improves outcomes of our patients, but it has another very important effect: The 20 residents who graduate as gynaecologists from Mulago Hospital every year, will take their vacuum extraction skills to all parts of Uganda, making it the routine procedure it should be.
Conclusion:
This study shows two things:
1: Use of vacuum extraction improves perinatal (and probably maternal) outcomes.
2: Teaching a skill to the many residents in a university hospital has a huge impact, probably even in other parts of the country.
Future plans:
In September 2014 we will intensify the program by training the 50 intern doctors in the department of obstetrics and gynaecology as well. We expect the vacuum extraction rate to increase further, but more importantly, we expect that those interns will take their skills to even more hospitals outside Kampala. Furthermore we will support the newly graduated gynaecologists who have started to work in other hospitals with equipment and teaching materials as they have notified us of their intention to use and teach vacuum extraction in their new hospitals.

|
|
